Ambetter Provider Reconsideration and Claim Dispute Form
This document is essential for providers looking to request a reconsideration or dispute a claim with Ambetter from Coordinated Care. It outlines the process, required information, and submission guidelines. Ensure to follow the instructions for a smooth submission and resolution.
Edit, Download, and Sign the Ambetter Provider Reconsideration and Claim Dispute Form
Form
eSign
Add Annotation
Share Form
How do I fill this out?
To fill out this form, start by gathering all necessary information such as your provider name, tax ID, and claim details. Ensure that you provide accurate information in each required field to avoid delays. After completing the form, submit it according to the provided instructions.
How to fill out the Ambetter Provider Reconsideration and Claim Dispute Form?
1
Gather all required information including provider details.
2
Select the level of dispute and reason for dispute.
3
Complete the requestor information section.
4
Attach any necessary supporting documents.
5
Submit the completed form to the appropriate address.
Who needs the Ambetter Provider Reconsideration and Claim Dispute Form?
1
Healthcare providers who have disputes with claims processing.
2
Billing departments seeking to rectify denied claims.
3
Medical offices needing clarification on claim payments.
4
Providers looking to appeal for reconsideration after claim denials.
5
Providers who need to address payment discrepancies.
How PrintFriendly Works
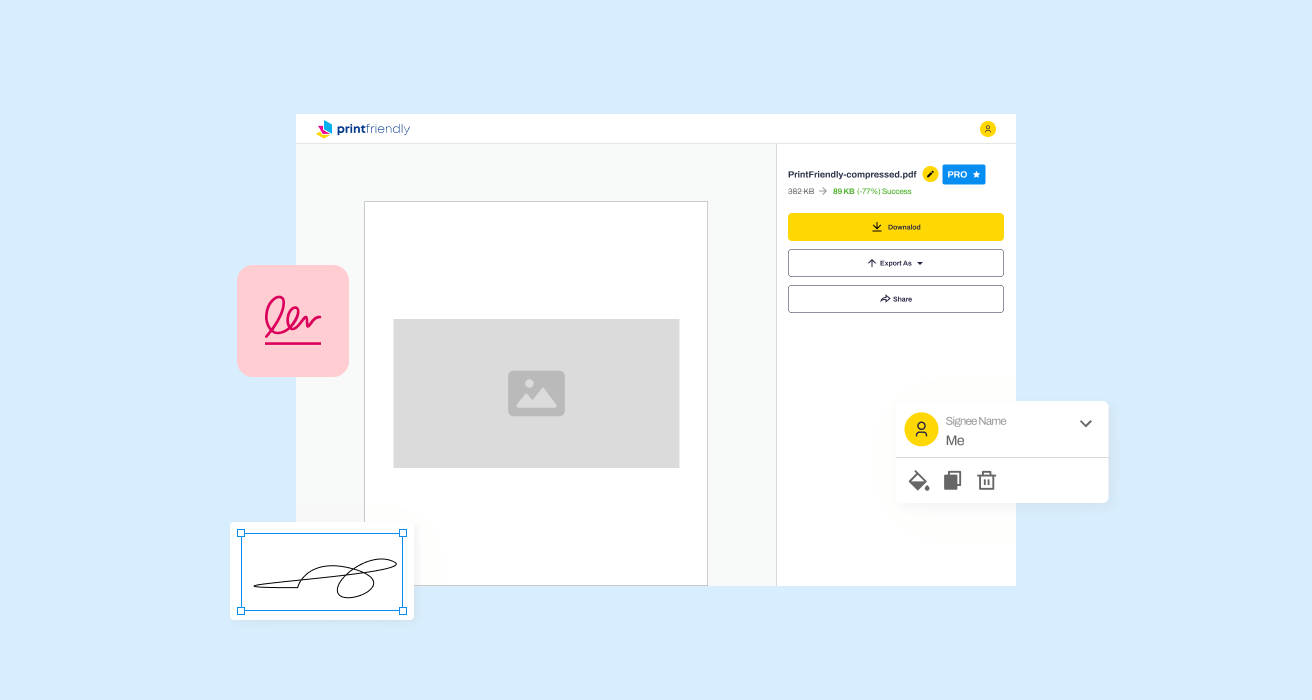
At PrintFriendly.com, you can edit, sign, share, and download the Ambetter Provider Reconsideration and Claim Dispute Form along with hundreds of thousands of other documents. Our platform helps you seamlessly edit PDFs and other documents online. You can edit our large library of pre-existing files and upload your own documents. Managing PDFs has never been easier.
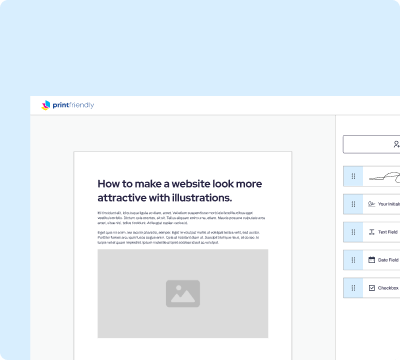
Edit your Ambetter Provider Reconsideration and Claim Dispute Form online.
Explore the new PDF editing functionality on PrintFriendly to easily modify this form. With intuitive tools, you can edit text, add notes, and highlight important sections. Tailor the document to suit your needs before sending it.
Add your legally-binding signature.
Now you can effortlessly sign PDFs on PrintFriendly. Simply navigate to the PDF, click the signature option, and draw or type your signature. This feature ensures your submissions are officially endorsed.
Share your form instantly.
PrintFriendly allows you to share PDFs with ease. You can quickly generate a shareable link to this document, making it accessible for colleagues and staff. Collaborate efficiently by sharing the PDF directly from our platform.
How do I edit the Ambetter Provider Reconsideration and Claim Dispute Form online?
Explore the new PDF editing functionality on PrintFriendly to easily modify this form. With intuitive tools, you can edit text, add notes, and highlight important sections. Tailor the document to suit your needs before sending it.
1
Open the document in PrintFriendly's PDF editor.
2
Select the text you wish to edit and make changes.
3
Use the annotation tools to add comments or highlights.
4
Review your edits to ensure all information is correct.
5
Download the edited PDF to keep your changes.

What are the instructions for submitting this form?
To submit this form, mail the completed document along with any supporting documents to the designated address for Level I or Level II disputes. For Level I, send to: Ambetter from Coordinated Care, Attn: Level I - Request for Reconsideration, PO Box 5010, Farmington, MO 63640-5010. For Level II, send to: Ambetter from Coordinated Care, Attn: Level II - Claim Dispute, PO Box 5000, Farmington, MO 63640. Consider sending via trackable mail for confirmation of receipt.
What are the important dates for this form in 2024 and 2025?
Ensure submissions for reconsideration or disputes are made within 24 months from the original EOP or denial date. Important dates for 2024 and 2025 will be relevant when planning claim disputes. Check for any updates on policy changes that might affect these timelines.

What is the purpose of this form?
The purpose of this form is to allow healthcare providers to formally request a reconsideration of denied claims or to dispute claims that have not been processed correctly. By providing a clear and structured means to communicate with Ambetter from Coordinated Care, providers can address issues that impact their practice and revenue cycle. This form is crucial for maintaining effective communication between providers and the insurance company.
Tell me about this form and its components and fields line-by-line.
- 1. Provider Name: Enter the full name of the healthcare provider.
- 2. Provider Tax ID #: Include the tax identification number associated with the provider.
- 3. Control/Claim Number: Provide the control or claim number related to the dispute.
- 4. Date(s) of Service: Specify the date(s) when the service was rendered.
- 5. Member Name: Enter the name of the member associated with the claim.
- 6. Member (RID) Number: Include the member's RID number provided by the insurance.
- 7. Level of dispute: Select whether this is a Level I Request for Reconsideration or Level II Claim Dispute.
- 8. Reason for Dispute: Indicate the reason for the claim dispute by checking the appropriate box.
- 9. Requestor Name: Provide the name of the individual submitting this request.
- 10. Requestor Phone Number: Enter a phone number where the requestor can be reached.
- 11. Date of Request: Date on which the request is being submitted.
What happens if I fail to submit this form?
Failure to submit this form can result in unresolved claim discrepancies, forcing you to bear financial losses. Claims may remain denied without an official request for reconsideration or dispute. It's crucial to adhere to submission deadlines to ensure your issues are addressed properly.
- Delayed Payments: Without submission, claims will not get resolved, causing payment delays.
- Unresolved Disputes: Filing is essential for formally addressing issues; otherwise, they may linger.
- Loss of Revenue: Denial of claims can lead to significant income losses for providers.
How do I know when to use this form?
- 1. Dispute Denied Claims: Use this form to challenge decisions on claims that have been denied.
- 2. Request Reconsideration: Formalize a request for revising the outcomes related to claim processing.
- 3. Correct Payment Issues: Address any discrepancies regarding payment amounts or incorrect provider payments.
Frequently Asked Questions
How do I submit the Claim Dispute form?
Submit the completed form by mail or fax to the addresses provided. Ensure all required fields are filled out completely.
What information is necessary to fill out the form?
You will need your provider name, tax ID, member details, and reason for the dispute.
Can I edit the PDF form before submitting?
Yes, you can use PrintFriendly to edit the PDF directly.
What happens if I miss the deadline for submission?
Timely submission is essential. Late submissions may be rejected based on the claims processing rules.
Is there a limit to how many disputes I can file?
There is no limit, but each claim must be eligible for reconsideration or dispute.
Can I attach supporting documents?
Yes, always include relevant documentation to support your claims.
Where can I find the mailing address?
The mailing address is included in the form instructions at the bottom.
What if my claim is still denied after reconsideration?
You may proceed to submit an appeal with additional documentation.
How can I check the status of my dispute?
You can check your claim status by contacting Ambetter customer service after submission.
What if I need assistance filling out the form?
Customer support is available to provide guidance on completing the form.
Related Documents - Ambetter Claim Dispute Form
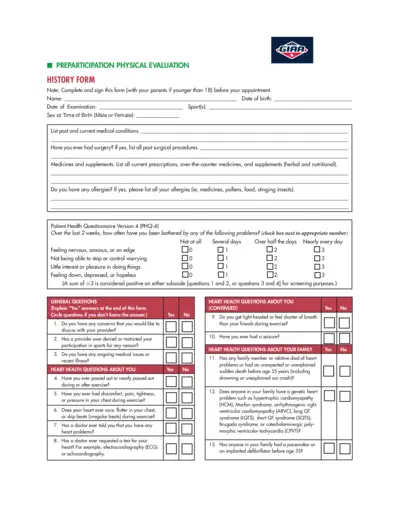
Preparticipation Physical Evaluation Form
The Preparticipation Physical Evaluation Form is used to assess the physical health and fitness of individuals before they participate in sports activities. It covers medical history, heart health, bone and joint health, and other relevant medical questions.
Health Insurance Tax Credits Guide 2015
This document provides a comprehensive guide on health insurance and premium tax credits for the 2015 tax year. It explains the tax filing rules, eligibility criteria, and detailed instructions for claiming and reporting premium tax credits. Essential for individuals who bought health insurance through the ACA Marketplaces.
TSP-77 Partial Withdrawal Request for Separated Employees
The TSP-77 form is used by separated employees to request a partial withdrawal from their Thrift Savings Plan account. It includes instructions for completing the form, certification, and notarization requirements. The form must be filled out completely and submitted along with necessary supporting documents.
Ray's Food Place Donation Request Form Details
This file contains the donation request form for Ray's Food Place. Complete the general information section and follow the guidelines to submit your donation request at least 30 days in advance. The form includes fields for organization details and donation specifics.
Pastoral Ministry Evaluation Form for Board of Elders
This evaluation form is designed for the Board of Elders to assess and provide feedback on a pastor's ministry. It aims to offer affirmation and identify areas for improvement. The form covers preaching, worship leading, pastoral care, administration, and more.
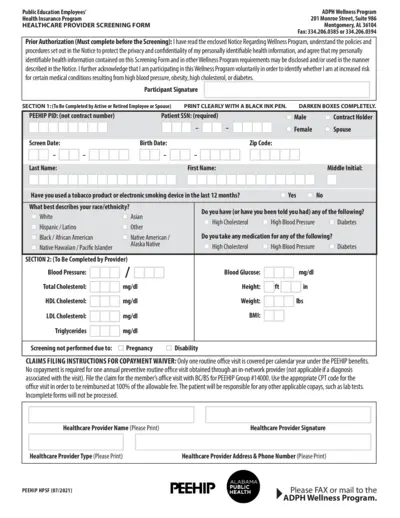
Health Provider Screening Form for PEEHIP Healthcare
This file contains the Health Provider Screening Form for PEEHIP public education employees and spouses. It includes instructions on how to fill out the form for wellness program participation. The form collects personal, medical, and screening details to assess wellness.
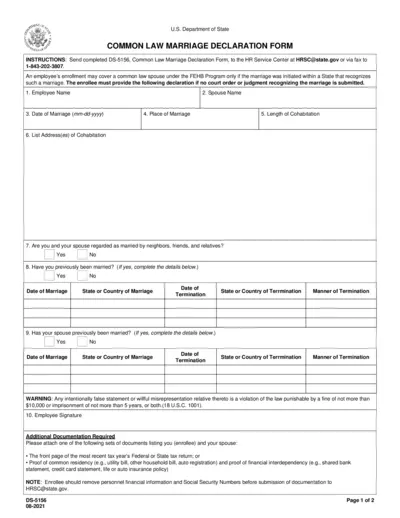
Common Law Marriage Declaration Form for FEHB Program
This form is used to declare a common law marriage for the purpose of enrolling a spouse under the Federal Employees Health Benefits (FEHB) Program. It requires personal details, marriage information, and additional documentation. Submission instructions and legal implications are included.
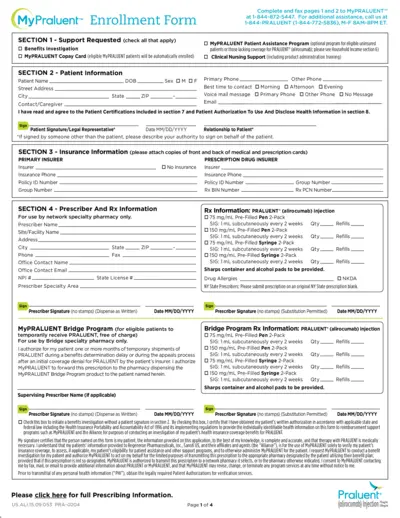
MyPRALUENT™ Enrollment Form Instructions and Details
This document provides comprehensive instructions and details for enrolling in the MyPRALUENT™ program, including benefits, patient assistance, and clinical support. It outlines the required patient, insurance, and prescriber information, as well as the steps for treatment verification and household income documentation.
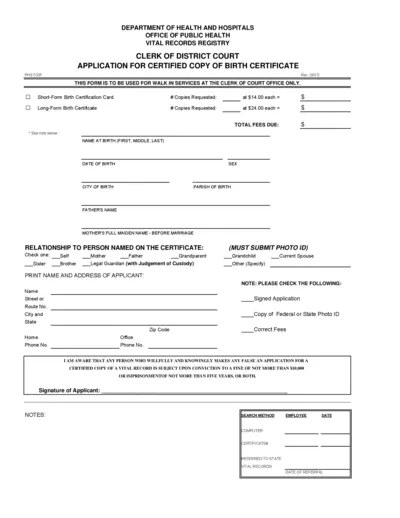
Application for Certified Copy of Birth Certificate
This form is used to request a certified copy of a birth certificate from the Clerk of Court Office. It includes details about the applicant, the person named on the certificate, and requires a photo ID and the correct fee. This form is only for walk-in services.
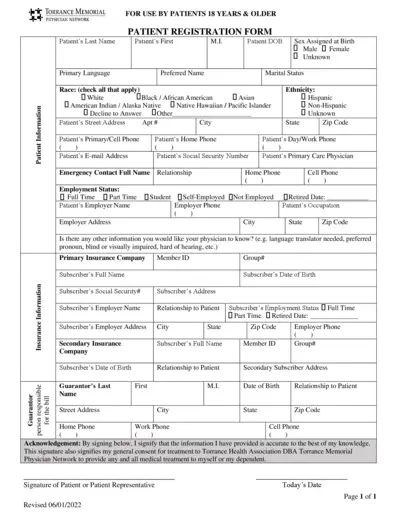
Torrance Memorial Physician Network Forms for Patients 18+
This file contains important forms for patients 18 years and older registered with Torrance Memorial Physician Network. It includes patient registration, acknowledgment of receipt of privacy practices, and financial & assignment of benefits policy forms. Complete these forms to ensure your medical records are up-to-date and to understand your financial responsibilities.
Vodafone Phone Unlocking Guide: Steps to Unlock Your Phone
This guide from Vodafone provides a step-by-step process to unlock your phone. Learn how to obtain your unlock code by filling out an online form. Follow the instructions to complete the unlocking process.
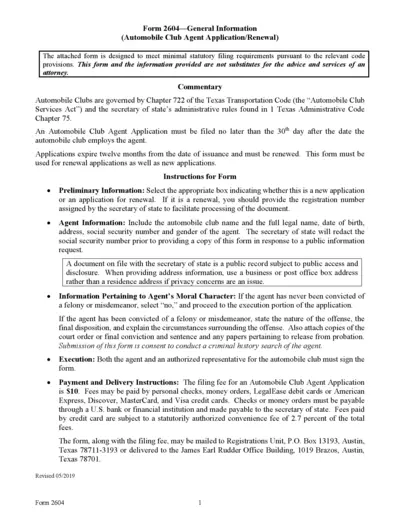
Texas Automobile Club Agent Application Form
This file is the Texas Automobile Club Agent Application or Renewal form, which must be submitted within 30 days after hiring an agent. The form includes fields for agent identification, moral character information, and requires signature from both the agent and an authorized representative of the automobile club. Filing fees and submission instructions are also provided.